Your Brain on Trauma
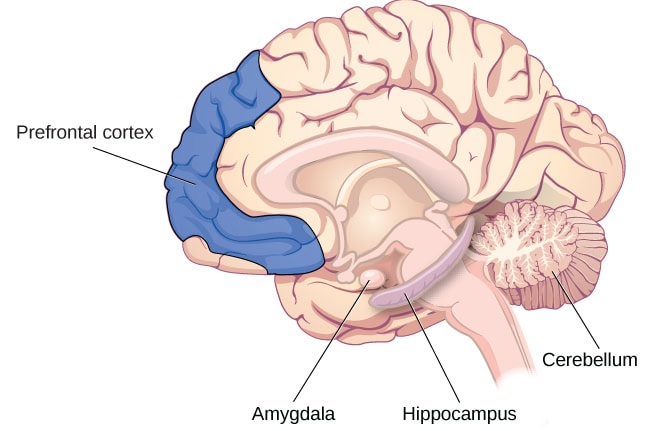
Kids who have experienced trauma often live in a state of hyperarousal or hypoarousal, in which their day-to-day lives can feel like they are in survival mode. We now understand that chronic childhood trauma causes negative impact and inflammation to the limbic system, the brain area in charge of emotions, relation, and connection.
When we experience trauma, our brain shuts down all nonessential systems. This means the prefrontal cortex that controls rational thinking and regulates emotions becomes muted. The limbic system, which includes the hippocampus and the amygdala, activates the sympathetic nervous system, which then prepares our body to respond to a perceived threat. Childhood Trauma Heal Through Positive Relationships
Our body releases a flood of hormones to boost alertness and heart rate which sends extra blood to the muscles. Our breathing gets faster to bring fresh oxygen to the brain and glucose into the blood for energy. We are prepared for fight, flight, freeze, or fawn. Childhood Trauma
PTSD occurs when the brain gets stuck in this response pattern. The prefrontal cortex also decreases in volume when the amygdala is overactivated.
The hippocampus sits below each temporal lobe near our ears, and is the memory center, responsible for memory formation and differentiating between past and present. The hippocampus stores memories, learning, and navigation, and also makes sense of trauma experiences. When functioning normally it calms the amygdala alarm circuit.
When we are triggered—reminded of a traumatic event by smells, sounds or other stimuli—our brain goes down a well-worn trail that’s called our trauma response. The trauma response may look different between individuals. For some, it may be anger, aggression, emotional outbursts and for others it may be shutting down, disassociating, and feeling numb. The good news is that we can teach our brain to renavigate, to take another path, and build different habits. This is the miracle of
neuroplasticity, or the brain’s ability to heal itself. We can facilitate neuroplasticity through healthy and trusting relationships and with positive skill building to manage triggering events and emotions. We then build new positive experiences that begin to override the negative memories and experiences. It’s never too late to help someone learn how to live outside of their traumatic experiences.
THE TRAUMA-INFORMED ENVIRONMENT
HEALING FROM TRAUMA BEGINS WITH A FOUNDATION OF REAL AND FELT SAFETY
Students arriving at Sierra Sage Treatment Center experience trauma-informed care in every aspect of their stay from those first few hours through graduation day. The Rite of Passage Integrated Care Model begins with a foundation of safety, explores strengths and needs of the individual, then teaches and reinforces necessary skills, before youth arrive at goal attainment. Each path to those goals is as unique as the person.
“When kids first come to our treatment center, we need to go slow and easy,” explains Program Director Rebekah Graham. “We make sure their human needs are met and we only focus on essentials that day.” This includes assessments, introductions, a tour of the campus, being connected to a mentor, and meeting therapy dogs Clark and Gogo.
Most girls arrive at Sierra Sage in a state of hypervigilance, exhibiting extreme awareness of any perceived threats to safety like loud noises or sudden movements. Graham and her team create an environment of real and felt safety through the physical environment and structured daily schedules. Once new students know what to expect they begin to relax and take steps toward healing.
A trauma-informed environment means low sensory input with high emotional and behavioral support. There are round fuzzy “take ten chairs” everywhere on campus for youth to use when they are feeling overwhelmed. “This gives them an appropriate option to check out and learn how to self-regulate,” says Graham.
The Sierra Sage campus also has “comfort rooms” decorated in pastel colors, with comfortable chairs and low lighting. Youth can go to these rooms of their own initiative, use coping skills from their soothing plan, and rejoin the group when they’re ready. Giving youth choices in the context of structure and routine is an important part of the Integrated Care Model because it gives kids a sense of agency and encourages them to take ownership of their individual healing process.
A Message From Christine Gwin, LCSW Regional Clinical Director
Many people can define what trauma is, but the challenge is understanding what trauma looks like for the youth we serve. Statistics estimate more than seventy-five percent of youth in the child welfare and juvenile justice systems have experienced at least one traumatic event, but during the assessment process we find that many don’t even recognize their experiences as being traumatic or display textbook symptoms that typify trauma survivors. Often their trauma responses are behaviors that are labeled “delinquent,” like aggression, self-harm, defiance, drug and alcohol dependence, among others. Our youth have learned how to adapt to their environments to achieve their definition of survival. Our goal is to help them process their trauma, learn effective ways to manage their symptoms, and replace their survival trauma responses with healthy coping skills.

Healing doesn’t start in the therapy room. If it takes a village to raise a child, the same is true for helping them heal. This begins in the milieu with a “village” of direct care staff who establish safe and caring relationships with each youth. Our Integrated Care Model, a trauma-responsive framework, informs the process of healing through a multi-disciplinary approach. Therapists, teachers, counselors, clinicians, placing agencies, and parents or guardians form a group of caring adults tasked with understanding the needs and strengths of each youth and supporting their treatment journey. For many youth these connections might be some of the first safe relationships they have ever had the opportunity of forming.
Our programs encourage youth to set daily goals of developing and practicing important skills that will help them succeed within their treatment and within their lives. Through cognitive and dialectical behavioral therapy, in tandem with adjunct treatment, such as EMDR, meditation, yoga, art/drama, and animal-assisted therapy, youth overcome past traumas and develop healthy coping mechanisms. When youth set and reach goals and treatment milestones, they learn that their trauma experiences don’t have to define their future.
This article, The Brain’s Response to Childhood Trauma and How to Heal Through Positive Relationships, was originally written as an article, Your Brain on Trauma, in our 2023 Rite of Passage Magazine. To read the full magazine please click here.